
Browning Laboratory
Darren D. Browning PhD
Professor, Department of Biochemistry & Molecular Biology
Member of the Georgia Cancer Center
Director, Biochemistry and Cancer Biology Graduate Program
Medical College of Georgia
Augusta University, Augusta, GA
Dr. Darren Browning earned his PhD in Cellular and Developmental Biology at the University of Toronto in Canada in 1995. He then moved to the Department of Immunology at The Scripps Research Institute in La Jolla, California to carry out his post-doctoral training. In 1999 he joined the Department of Pharmacology at the University of Illinois at Chicago, where as research faculty he developed an independent research program focusing on cGMP-dependent protein kinases. In 2001 Dr. Browning joined the Department of Biochemistry and Molecular Biology in the Medical College of Georgia at Augusta University, and has risen through the ranks and became a full professor in 2013. He has been actively engaged in education and teaches biochemistry to 1st year medical students and graduate students, and he has served as Director of the Graduate Program in Biochemistry and Cancer Biology since 2003.
The focus of Dr. Browning’s laboratory continues to be on cyclic-GMP signaling, and he is an internationally recognized expert on the cGMP-dependent protein kinases (PKG). He has published over 50 papers in top journals, including several invited review articles. His work has been funded by the Arthritis Foundation, Georgia Cancer Coalition, American Cancer Society, and currently the National Cancer Institute of the NIH. The present focus is on therapeutic effects of activating cGMP signaling in the colon mucosa. His laboratory has found that FDA-approved phosphodiesterase inhibitors can increase cGMP levels in the colon mucosa, and that this is chemopreventative for colon cancer, and is therapeutic for ulcerative colitis and constipation and in preclinical models. Dr. Browning interacts regularly with clinical faculty in the Digestive Health Center, and with pharmaceutical companies (Ironwood and Synergy) to further the long term goal of understanding the signaling mechanisms and translational potential to benefit human patients.
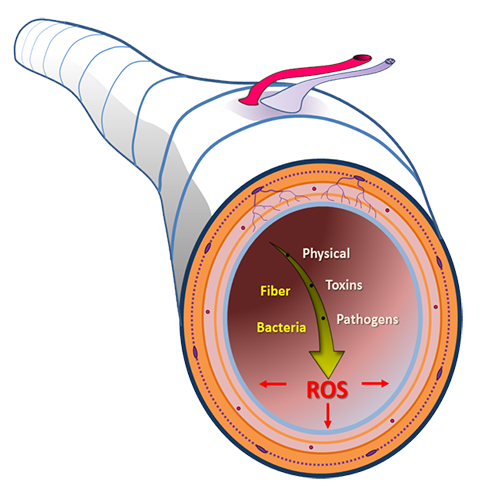
The Browning laboratory was the first to report that clinically available erectile dysfunction drugs are able to increase cGMP levels in the gut epithelium and that this is barrier-protective and can block experimental colitis in normal (wild type) mice. The signaling pathways downstream of cGMP are an area of current interest in the laboratory, and they have identified that regulation of homeostasis by type 2 cGMP-dependent protein kinase signaling plays a central role. Further, they have evidence that PKG2 regulates stress pathways to protect the lining of the colon from oxidative damage, and a current focus is on the activation of FoxO transcription factors.
Exploiting cGMP signaling for the treatment of gastrointestinal diseases
Irritable Bowel Syndrome (IBS)
Affects 10 million Americans (20%) experience
signs (5-15% of all children).
Principally neuromuscular, abdominal pain, cramping, along with diarrhea (IBS-D; 1/3), constipation (IBS-C),
or both (IBS-M).
Inflammatory Bowel Disease (IBD)
Affects 1.6 million Americans, (80,000 are children).
Damaging inflammation (includes Crohn's and Ulcerative Colitis). Abdominal pain and frequent, severe, and
bloody diarrhea.
Colorectal Cancer (CRC)
Affects 1.3 million Americans (have or are survivors), 150,000 will be diagnosed and 50,000 will die per year in
the USA. Metastatic disease is usually lethal due to a few effective treatments. Chemoprevention is warranted for some populations.
The most common and severe diseases affecting the colon are a focus of our work.
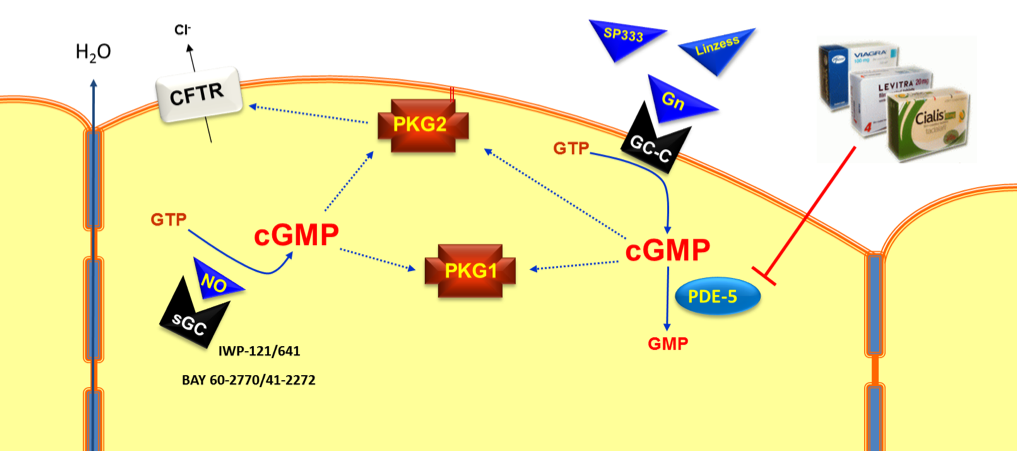
Drugs that can target the cGMP signaling axis in luminal epithelial cells of the colon.
LABORATORY DISCOVERY IN THE NEWS:
We recently discovered that activating cGMP signaling in the intestinal epithelium using a low dose of the PDE5 inhibitor sildenafil significantly reduces intestinal tumors in mice.
Cover art for the journal “Cancer Prevention Research”:
Media Articles: