May 2025
70Year-old Female with Left Thigh Redness and Pain
Author: Benjamin Caviston, MD PGY-3
Peer Reviewers: Lee LaRavia, DO; Dan Kaminstein, MD
Learning Objectives:
- List/discuss DDX of Skin/Soft tissue Infections
- Discuss use of US in the workup
- Discuss the US characteristics/findings associated with NSTI
- Review of recent literature regarding POCUS in diagnosis of NSTI
Case Presentation
- 70F with history of lung cancer on immunotherapy presents with 1 day of progressive left thigh redness/pain. Noticed pain and redness to medial thigh which has rapidly progressed over course of the day, now has area of central bruising
- T: 36.9 °C (Oral) HR: 96(Peripheral) RR: 24 BP: 101/73 SpO2: 100% WT: 53.200 kg
- Exam: Large area of erythema, warmth, induration to the left medial thigh, central area of ecchymosis, No Crepitus, No Knee effusion
- DDx: Necrotizing Fasciitis, Cellulitis, Erysipelas, Abscess, Pyomyositis, Septic Arthritis, Deep Venous Thrombosis, Superficial Thrombophlebitis
Differential Diagnosis
- Pulmonary: Asthma/COPD. Pneumonia, pneumothorax
- Cardiogenic: PE, ACS/MI, CHF, cardiomyopathy, dysrhythmia, cardiac tamponade, valvular disease, post-viral peri/myocarditis
- Other: Cancer, Tuberculosis, HIV, Chagas, Endomyocardial Fibrosis (EMF), Schistosomiasis, hookworm, syphilis, Rheumatic heart disease
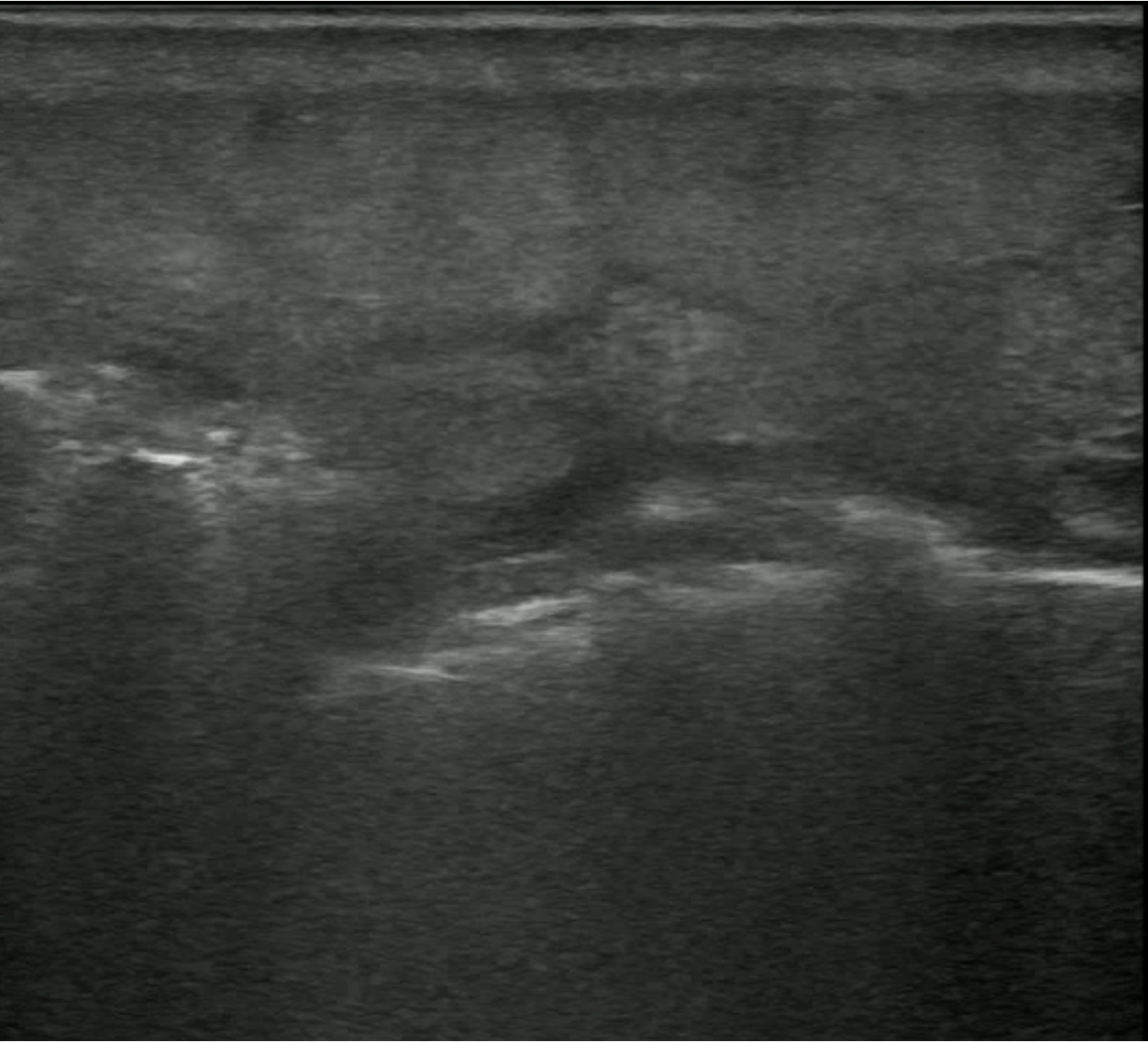
POCUS Images
- Medial Thigh Soft Tissue
POCUS Interpretation
- Cobblestoning: Fat lobules separated by hypoechoic fluid (Blue arrows)
- Seen in any cause of tissue edema
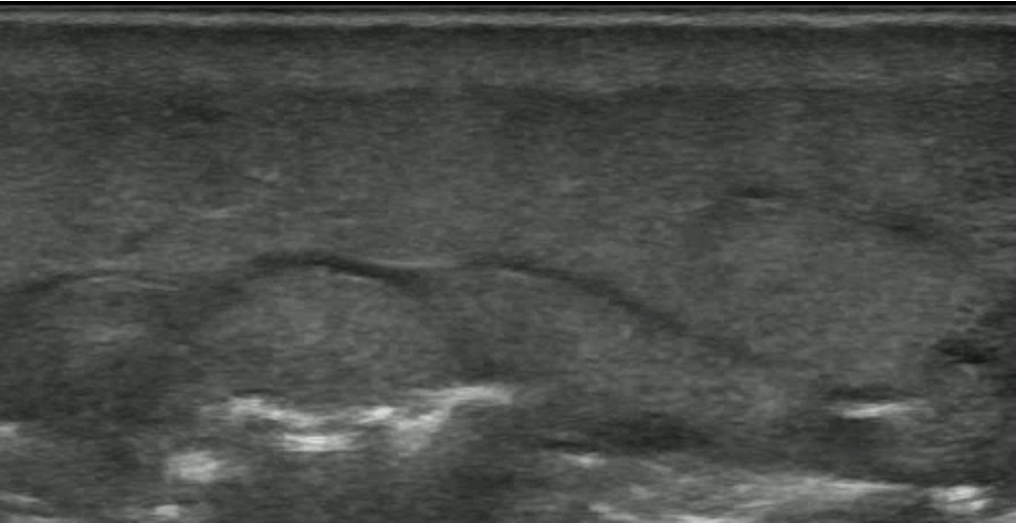
- Hyperechoic lines (Red Arrow) with dirty white shadowing (Green Arrows)
- This Finding is suggestive of gas within the Soft Tissues
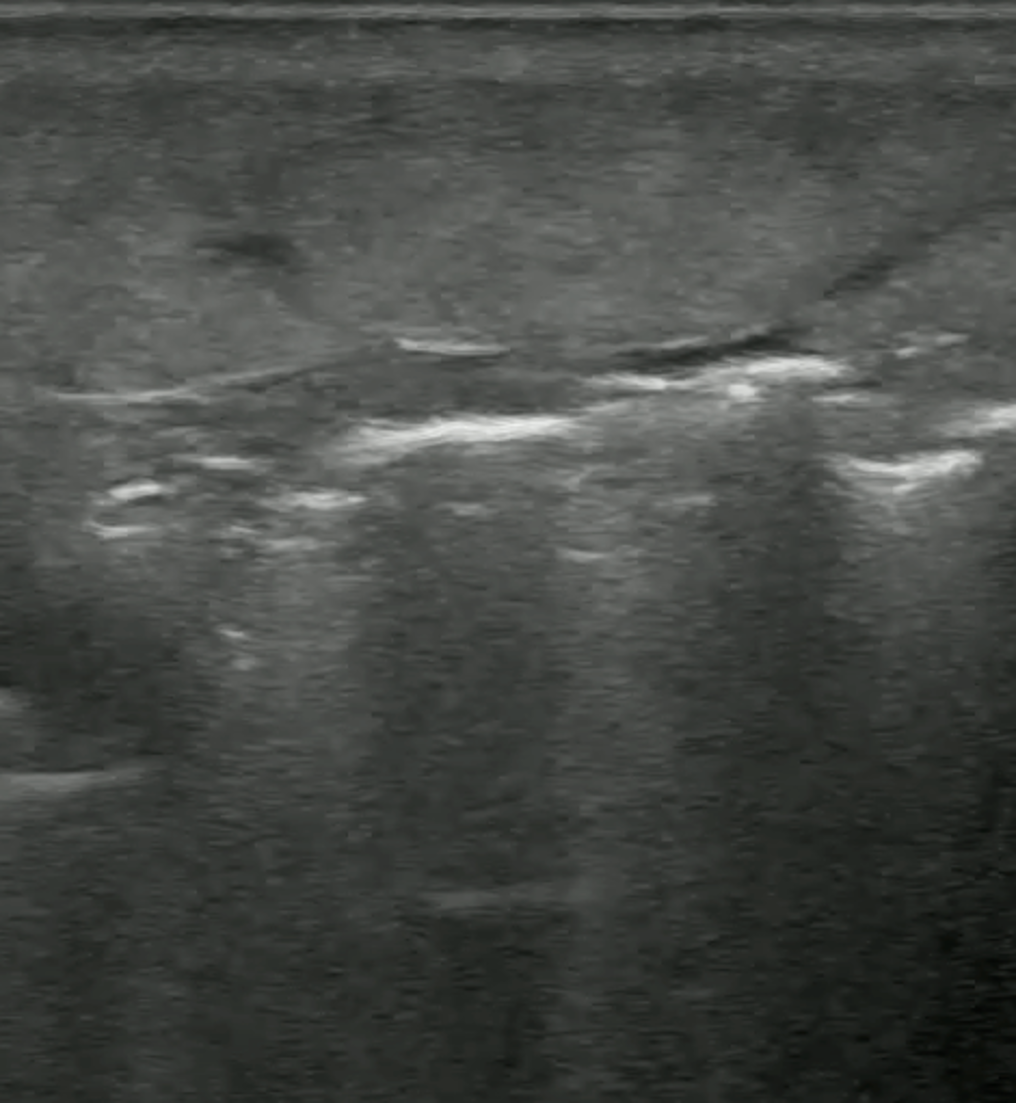
- Fluid Stripe along Fascial Plane
Diagnosis and Case Disposition
- This patient had Necrotizing Fasciitis of the Thigh
- Surgery was consulted and agreed to operate based on exam and POCUS before any labs and formal imaging could be completed
- Unfortunately Patient rapidly decompensated and went into Cardiac Arrest before being taken to OR
- Blood Cultures ultimately grew Clostridium Septicum
Pathophysiology and Diagnosis
- Rapidly progressive infection along fascial planes
- Typically Polymicrobial
- Anaerobes: Clostridium
- Gram Positives: Streptococcus (GAS), Staphylococcus (MRSA)
- Gram Negative: Pseudomonas, Klebsiella, Vibrio Vulnificus
- Most sensitive diagnostics are CT and MRI but both have low specificity (Tso 2018)
- CT Sensitivity 80%
- MRI Sensitivity 93%
Literature Review
- Castleberg et al 2014; Proposal of the STAFF Protocol, evaluating for S ubcutaneous T hickening, A ir and F ascial F luid to rule in Necrotizing Fasciitis
- Not Validated but is a useful mental framework
- Marks et al 2023; Systematic Review of imaging findings associated with necrotizing
fasciitis, only 3 studies and 221 cases included
- Fluid Accumulation: 85% Sensitive 45% Specific
- Thickened Fascia: 67% Sensitive 55% Specific
- Subcutaneous Gas: 6% Sensitive 100% Specific
- Lahham et al 2022; Prospective study (N=64) of patients presenting to ED with clinical
concern for NSTI, results of POCUS were compared to CT and Surgical findings sensitivity
of 100% and specificity of 98.2%
- Small study, Sensitivity/Specificity higher than prior studies, 100% of positive cases had presence of soft tissue gas which does not reflect reality
Take Away Points
- Necrotizing Fasciitis is an emergent and cannot miss diagnosis
- CT and MRI are the most sensitive studies (poor sensitivity) but delay time to diagnosis
- POCUS findings include gas within tissues and fluid along fascial planes
- US is useful to Rule-in the diagnosis of necrotizing fasciitis but ruling out should be done in conjunction with advanced imaging (CT or MRI), scoring systems and surgical consultation
- Consider routine use of POCUS in patients whose presentation is concerning for NSTI to facilitate rapid treatment and consultation
References
- Castleberg, E., Jenson, N., & Am Dinh, V. (2014). Diagnosis of necrotizing faciitis with bedside ultrasound: the STAFF Exam. Western Journal of Emergency Medicine, 15(1), 111.
- Lahham, S., Shniter, I., Desai, M., Andary, R., Saadat, S., Fox, J. C., & Pierce, S. (2022). Point of Care Ultrasound in the Diagnosis of Necrotizing Fasciitis. The American journal of emergency medicine, 51, 397–400. https://doi.org/10.1016/j.ajem.2021.10.033
- Marks A, Patel D, Sundaram T, Johnson J, Gottlieb M. Ultrasound for the diagnosis of necrotizing fasciitis: A systematic review of the literature. Am J Emerg Med. 2023 Mar;65:31-35. doi: 10.1016/j.ajem.2022.12.037. Epub 2022 Dec 22. PMID: 36580698.
- Tso D & Singh A. Necrotizing Fasciitis of the Lower Extremity: Imaging Pearls and Pitfalls. Br J Radiol. 2018;91(1088):20180093. doi:10.1259/bjr.20180093 - Pubmed