
- Augusta University
- Georgia Cancer Center
- Community Connections
- Women's Health on the Road
- Breast Cancer Screening
Breast Cancer Screening
![]()
What to expect on the screening day
Contact Us
Women's Health on the Road
Health Sciences Campus
GCC - M. Bert Storey Research Building
706-721-xxxx
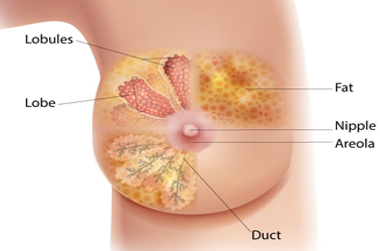
What is breast cancer?
Breast cancer happens when the cells in the breast change and grow out of control. Breast cancer affects 1 in 8 women in the U.S. and is the most common cancer in women. It is also a leading cause of cancer deaths. Because everyone has breast tissue, breast cancer can happen to anyone, but it is about 100 times more common in women than men.
Breast cancer is classified based on the type of cells where the cancer forms and whether it spreads.
- Invasive breast cancer – cancer cells have spread beyond the place where they first formed and can invade other parts of the body.
- Non-invasive breast cancer (in-situ)– abnormal cancer cells stay in the tissue where they formed and have not spread.
Why breast screening matters - Breast cancer screen saves lives!
Breast screening means checking a woman’s breast before signs or symptoms of disease
show up.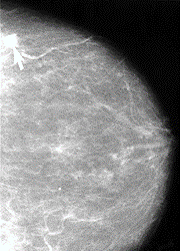
The goals of breast cancer screening are to:
- find cancer early when it is easier to treat and cure
- decrease the number of late-stage or severe cancers
- reduce the number of breast cancer deaths
What screening test is used for breast cancer?
One of the most used tests is a screening mammogram. A mammogram is a low-dose x-ray. The x-ray picture shows your breast tissue including any abnormal areas. Mammograms cannot show if an abnormal area is cancer, but they can help your healthcare provider decide if you need more tests. You can only get a screening mammogram before you have symptoms. Once you have any symptoms you will need a diagnostic test.
What to expect on the screening day
Follow these screening guidelines:
- Be informed.
- Know about the benefits and harms of screening tests.
- Talk with your doctor about breast screening and together decide which is the best screening test for you.
If you are a woman with average risk for breast cancer, follow these breast screening guidelines:
- 40-44 years – begin annual mammogram
- 40-74 years – mammogram every other year
 Groups with higher breast cancer risk
Groups with higher breast cancer risk
About 5-10% of breast cancers are hereditary. These are passed on through genes inherited from the parents. It is important to know your family’s history of cancer.
Women at higher risk for breast cancer include those with a family history of breast cancer such as a close blood relative (mother, sister, daughter) who had the disease.
Breast cancer is the leading cause of cancer death among African American/Black women. They also have a higher chance of getting aggressive breast cancer at younger ages. Black women are two times more likely to be diagnosed with triple negative breast cancer compared to White women. Dense breast tissue is more likely in Black women.
Regardless of gender, breast cancer can develop in any breast tissue. Estrogen used in hormone therapy can also increase the risk. Trans-men and trans-women should consider breast health as part of their routine health care and follow breast cancer screening guidelines even if they have not received hormone therapy.
The bottom line – You can reduce your risk of breast cancer!
As we age, the risk of breast cancer increases. We can reduce our risk of getting breast cancer by:
- Avoiding alcohol and heavy drinking
- Keeping a healthy weight for our height
- Being physically active – getting at least 30 minutes of exercise every day
- Not smoking and avoiding secondhand smoke exposure. If you smoke, get help quitting!
- Following breast cancer screening guidelines
For new mothers, feeding babies with breast milk helps protect against breast cancer. Encourage and support new moms in their efforts to breast feed or to pump breast milk at home and in the workplace.
About your screening day
How and when will I get the results of my mammogram?
You will get a letter with your results and can expect them in a few days after your visit. If you do not receive your results in 30 days, you can contact the patient navigator.
What do my mammogram results mean?
Healthcare providers use a standard system called Breast Imaging Reporting and Data System (BI-RADS) to describe mammogram results. The results are a numbered category from 0-6.
- 0- Incomplete: Additional imaging is needed
- 1- Negative: Normal result, nothing new or abnormal was found
- 2- Benign finding: No sign of cancer, but there was a non-cancerous finding
- 3- Probably benign finding: Low chance of being cancer, but you will likely need more imaging tests
- 4- Suspicious abnormality: May be cancer, breast biopsy recommended
- 5- Highly suggestive of malignancy: High chance of being cancer, breast biopsy strongly recommended
- 6- Known biopsy-proven malignancy: Previous biopsy has already shown cancer
Your mammogram report will also have information about your breast density, which is how much other tissue is in your breast compared to fatty tissue. Denser breasts make it harder to see abnormal areas on mammograms. It also slightly raises your risk of breast cancer.
What if I have a negative (normal) mammogram test result?
If you are 40 to 74 years old, mark your calendar to get screened every other year. If you are older than 74, talk with your doctor about next steps.
What if I have a result that is not negative or benign?
Your healthcare provider will share their recommendations with you. Depending on your result, they may recommend further testing. The good news is regular screening can catch breast changes and breast cancer early. Your health care provider is there to answer your questions, so be sure to ask!
Sponsors


Participating Clinics

