
- Augusta University
- Georgia Cancer Center
- Clinical Trials
- Never Say No
Never Say No
One of the most heartbreaking words a parent of a child with cancer can hear is “No.” No more treatment options to cure your child’s cancer. No more clinical trials to slow down the relapsed cancer. No more hope.
Here at the Georgia Cancer Center, our heart’s desire is to Never Say No. We are striving to offer a complete array of clinical trials to families looking for immunotherapy options for their child with relapsed cancer. And, as some of the world leaders in helping the immune system control cancer in children, who better to lead the way?
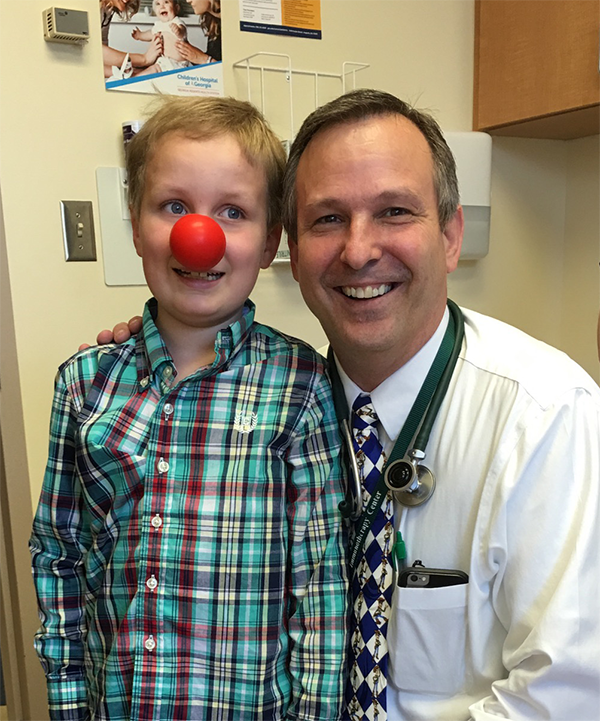
Overall, our immunotherapy clinical trials have treated over 100 patients with multiple different kinds of brain tumors, for which there would be no treatment expected to provide a cure. This includes more than a dozen patients with newly diagnosed Diffuse Intrinsic Pontine Glioma (DIPG), the very worst kind of brain tumor for which there is no curative therapy; these especially sick patients received chemotherapy/radiation/immunotherapy regimen as their front-line treatment, immediately upon diagnosis. We have seen some children with complex relapsed brain tumors have dramatic improvement in symptoms. Typically, an improved quality of life is not the expectation for children with relapsed brain tumors who enroll in experimental Phase I therapy trials. However, we have found that a number of the children receiving immunotherapy treatment are demonstrating quality of life improvements, such as returning to school, taking long-delayed vacation trips, engaging in activities they cherish such as hiking and rock climbing, moving in to a dormitory at college, attending sporting events, and more.
Contact Us
Jane Barrett
Health Sciences Campus
GCC - M. Bert Storey Research Building
1120 15th Street, CN-2224
Augusta, GA 30912
(706) 721-7398
The Time for Yes
Our heart’s desire is to Never Say No. Rather, we strive to say, “Yes, there are more treatment options to help your children’s cancer. Yes, there are clinical trials to slow down the relapsed cancer. Yes, there is more hope.”
Our vision is to offer a complete array of clinical trials to families looking for immunotherapy options for their child with cancer.
IDO: Groundbreaking Discovery
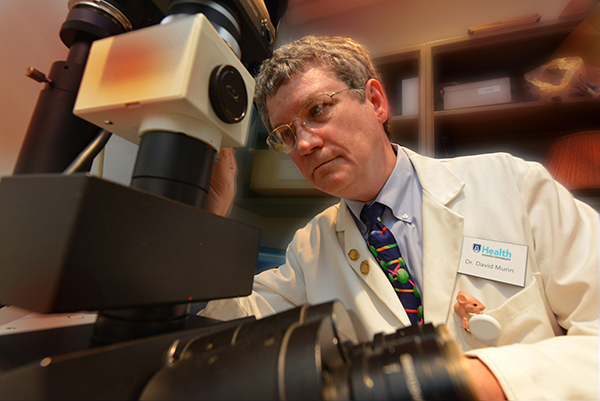
IDO is the abbreviation for the enzyme at the heart of the discoveries that started the pediatric immunotherapy program at the Georgia Cancer Center. Immunotherapy is a treatment approach to cancer that harnesses the power of the patient’s own immune system to attack the cancer.
In the 1990s, Dr. David Munn and his colleague, Dr. Andrew Mellor, discovered the role of IDO in protecting a fetus from being attacked by the mother’s immune system during pregnancy. Dr. Ted Johnson was involved as an MD/PhD student at the time. They realized that many tumors also use IDO to fool the immune system into tolerating rather than attacking the growing cancer; so, they developed drugs that block IDO. Augusta University obtained a patent on the findings - so that the drugs could be developed for clinical use - and partnered with the NewLink Genetics Corporation to speed up drug development.
One of those IDO-blocking drugs, Indoximod, is now in cutting-edge clinical trials for children with brain tumors at Augusta University. The use of Indoximod in brain tumors is based on Dr. Johnson’s work combining this drug with conventional cancer therapy (chemotherapy and radiation) to target brain tumors.
Treating More Pediatric Cancers
Based on preclinical laboratory results, the clinical trials are designed to test the concept that this class of drugs (IDO-inhibitor drugs) creates a synergy with standard treatments that makes the combined treatment work MORE POTENTLY against the brain tumor and requires lower doses of chemotherapy and radiation to achieve the more potent effect; therefore, the treatment may be LESS TOXIC and the children may have fewer side effects and BETTER QUALITY OF LIFE.
We have been able to design regimens that produce an excellent quality of life, with minimal well-tolerated side effects, yet still access the tumor-killing power of chemotherapy and radiation. Our ultimate goal is to achieve ten times the potency at one-tenth of the side effects.
Dr. Ted Johnson and Dr. David Munn have the following goals for quality-of-life features in all of their immunotherapy trials:
- Use oral medications whenever possible and focus on moderate doses of chemotherapy
- Have as much of the treatment as possible taken at home (keeping hospital stays to a minimum) and work closely with the referring centers to decrease the amount of travel for long-distance patients
- Use immunotherapy to help out the chemotherapy and radiation so that ultra-high doses can be avoided (important for minimizing side effects like nausea, vomiting, hair-loss, etc.)
- Focus on maintaining a good quality of life — the goal is to have children returning to school, playful and happy, not wiped-out and miserable
How to Make an Impact

Contribute
Seed funding for clinical trials to support launch of early-phase immunotherapy trials in children (data collection, sample collection, x-rays, etc.)

Give
Operating funds to continue nimble development of state-of-the-art new immunotherapy drugs for children, especially to quickly translate breakthroughs and opportunities into first-in children trials in childhood cancer.

Provide
Infrastructure support to add full-time, pediatric-focused personnel, including a pediatric nurse practitioner; oncology clinical-trials nurse-coordinator; data manager; and regulatory/compliance staff for first-in-children trials